Varicocele is a medical condition where the veins within the scrotum become enlarged, disrupting normal blood flow. This condition often develops over time and may not always show immediate signs, but its long-term effects can be significant. In particular, the relationship between varicocele and fertility has drawn increased attention due to its association with impaired sperm function and reduced chances of conception. As a correct understanding of this condition is vital, individuals should be aware of the potential health impacts and treatment options available.
This guide will explain what is varicocele, identify its signs, and answer common concerns such as can varicocele go away or can a varicocele cause infertility. You’ll also discover how varicocele symptoms may affect your quality of life, and why it’s essential to seek help if you suspect this condition. For couples facing reproductive challenges, it’s important to consider how varicocele infertility can influence the journey to parenthood. At our trusted Cyprus IVF clinic, we offer expert care for male reproductive issues as part of our holistic fertility approach. Whether you’re newly diagnosed or exploring your options, understanding treatment for varicocele can be the first step toward a healthier reproductive future.
What is Varicocele?
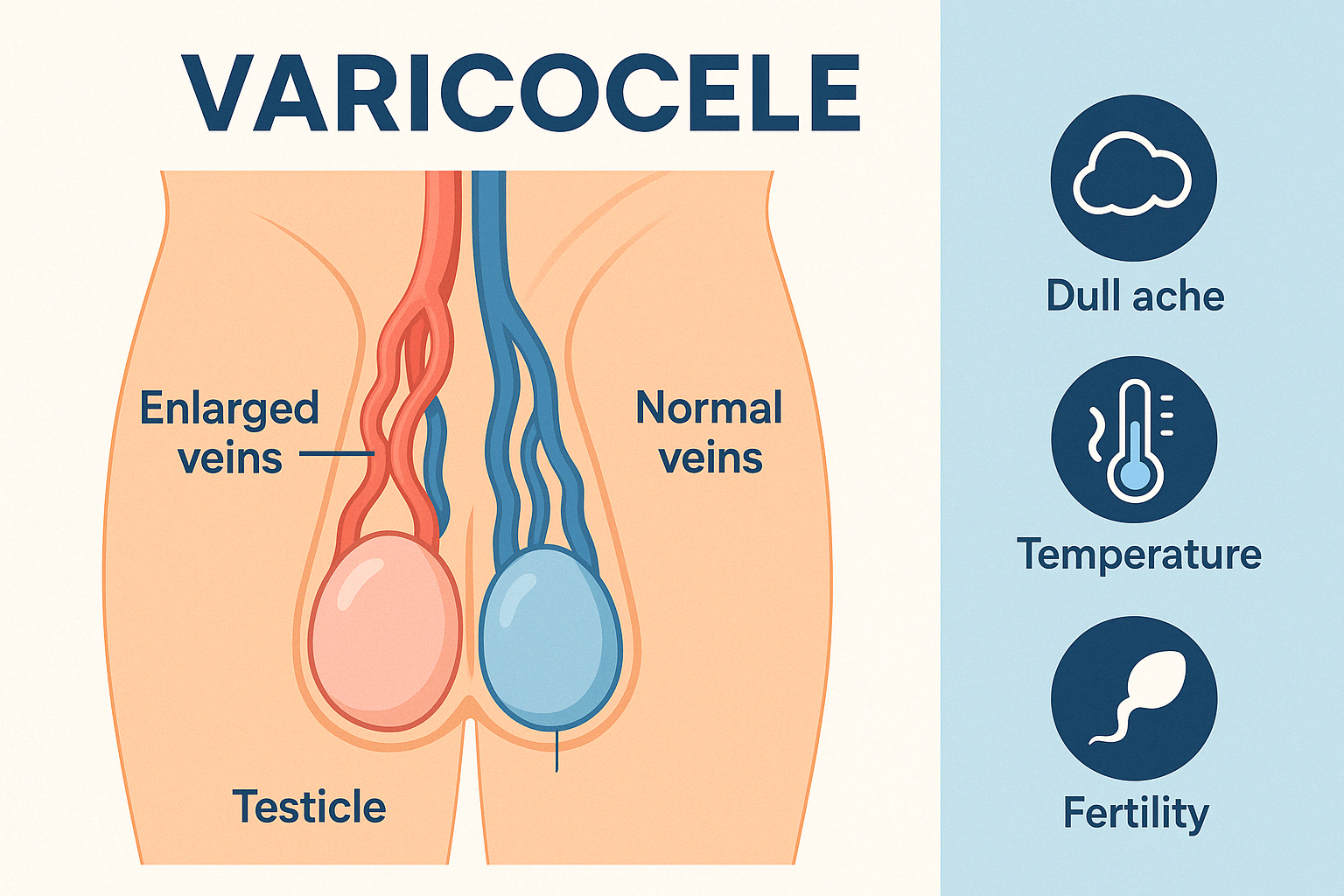
A varicocele is a medical condition characterized by the enlargement of the veins within the scrotum, specifically in the pampiniform plexus, which is responsible for draining blood from the testicles. This condition closely resembles varicose veins seen in the legs, but it occurs in the reproductive area and can directly influence male reproductive health. The exact mechanism involves the malfunction of valves within the veins, leading to blood pooling and increased pressure around the testicle. This often results in elevated scrotal temperature, which can disrupt normal sperm production. Because of these effects, understanding varicocele what is becomes important for any male experiencing fertility issues or scrotal discomfort.
Varicoceles typically form during puberty and develop slowly over time. Most cases are found on the left side of the scrotum due to anatomical reasons, although bilateral cases are also possible. In many instances, varicoceles do not cause noticeable symptoms and may only be discovered during a physical examination for infertility. However, when symptoms are present, they might include a dull ache, a visible or palpable lump, or a heavy feeling in the scrotum. If left untreated, the condition can impact sperm production and testosterone levels. Early detection and evaluation are key to determining the appropriate approach, especially for men considering fertility treatment such as IVF treatment in Cyprus.
How Common is Varicocele?
Varicocele is a relatively common condition, affecting approximately 15% of the general male population. Among men diagnosed with infertility, this percentage increases significantly—up to 40%. The condition most often develops during adolescence and continues unnoticed into adulthood unless it causes symptoms or fertility problems. Because of its silent progression, many men remain unaware they have it until undergoing a fertility evaluation or routine physical exam.
Research has shown that varicoceles are more prevalent on the left side of the scrotum due to anatomical reasons, though bilateral occurrences are not rare. The condition can affect men across all age groups but is particularly frequent in younger individuals, especially those between the ages of 15 and 25. Despite its prevalence, many cases are mild and asymptomatic, which can delay diagnosis and treatment. Early detection through physical examination and scrotal ultrasound is crucial, particularly for men planning to conceive.
What are the Types and Degrees of Varicocele?
Varicocele is classified into different types and degrees based on its anatomical location and how easily it can be detected during a physical examination. The two primary types are clinical varicocele and subclinical varicocele. Clinical varicoceles are palpable or visible upon physical exam, while subclinical varicoceles are not detectable by touch but can be diagnosed through imaging, such as Doppler ultrasound. Subclinical varicoceles typically present no symptoms and are often found during fertility assessments or scrotal ultrasounds performed for other reasons.
Varicocele severity is also graded in three main degrees:
- Grade 1: The varicocele is small and only detectable during a Valsalva maneuver (bearing down).
- Grade 2: The varicocele is moderate in size and palpable without the Valsalva maneuver.
- Grade 3: The varicocele is large and clearly visible through the scrotal skin.
These degrees help determine the level of vascular dilation and guide treatment decisions. The higher the grade, the more likely it may be associated with testicular discomfort or compromised sperm quality. For men facing reproductive challenges, identifying the grade of varicocele plays a crucial role in deciding whether surgical or other interventions are necessary. Understanding the degree can also provide insight into the potential impact on fertility, helping patients and physicians make informed decisions.
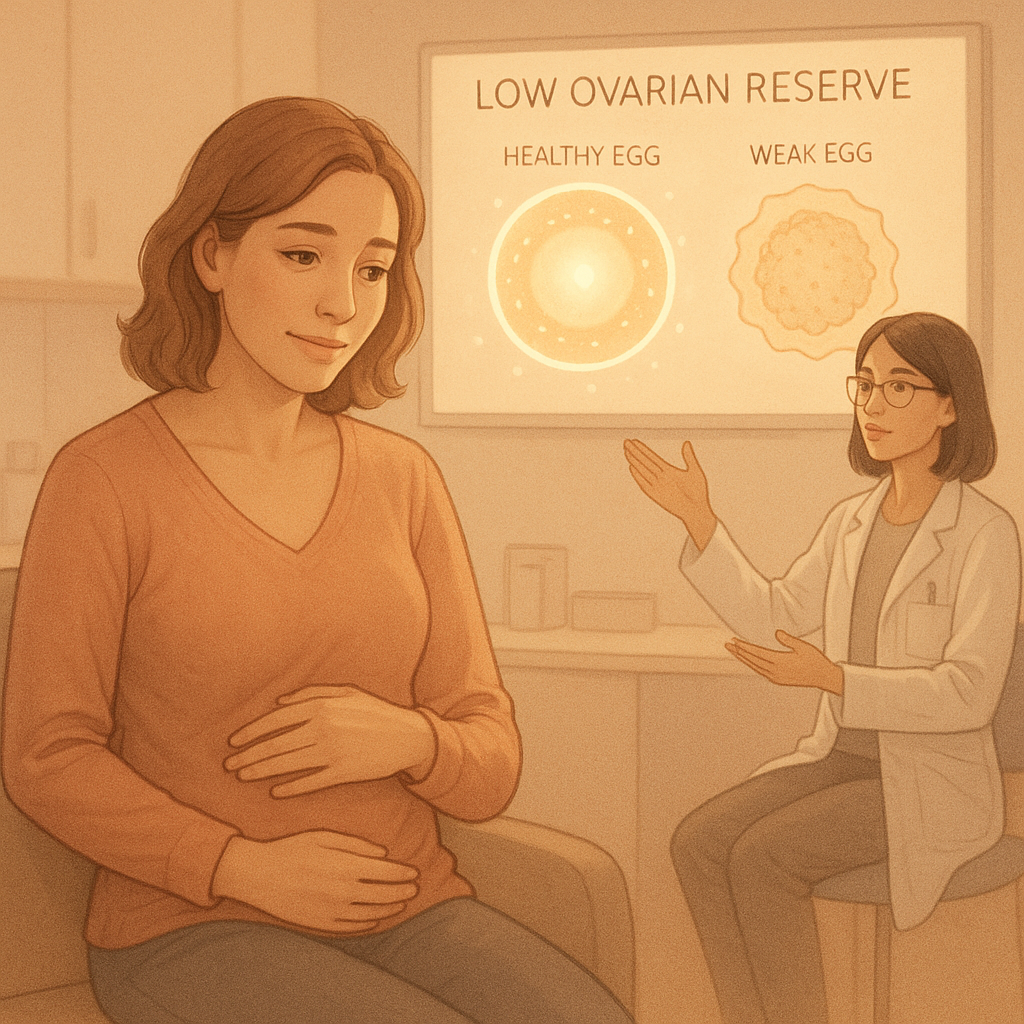
What are the Symptoms of Varicocele?
The symptoms of varicocele can vary greatly from person to person, with many individuals experiencing no noticeable signs at all. In asymptomatic cases, the condition is often discovered during routine check-ups or fertility assessments. However, when symptoms do appear, they typically include a dull ache or heaviness in the scrotum, particularly after prolonged standing or physical activity. This discomfort usually subsides when lying down. Some men may also notice enlarged veins in the scrotum that resemble a “bag of worms,” which can be a visible indication of varicocele.
In more severe cases, symptoms may be accompanied by testicular shrinkage or atrophy, as prolonged exposure to increased scrotal temperature can impair testicular function. Over time, this can negatively affect sperm production and hormonal balance. It is also common for men with varicocele to report decreased fertility or difficulty conceiving with their partner. Therefore, any ongoing scrotal discomfort or visible changes should be examined by a healthcare professional. Recognizing and addressing varicocele symptoms early is essential for preventing potential long-term effects on male reproductive health.
Physical Symptoms to Watch Out for
One of the most common physical signs of varicocele is a visible swelling or bulging vein in the scrotum, often described as a “bag of worms.” Other physical symptoms may include testicular asymmetry, heaviness, or a sensation of pressure in the groin area. These signs can worsen after exercise or prolonged standing, indicating possible cause varicocele.
Pain and Discomfort in the Scrotum
Men with varicocele often report a dull, aching pain in the scrotum that becomes more noticeable after physical activity or at the end of the day. This discomfort may feel like heaviness or pulling in the groin. Persistent pain could be an indication of underlying varicocele reasons and should be evaluated by a specialist.
Causes and Causes of Varicocele
The causes of varicocele are primarily related to malfunctioning valves within the veins that drain the testicles. Normally, these valves ensure that blood flows in one direction—from the testicles back toward the heart. When these valves fail, blood pools in the veins, causing them to dilate and form a varicocele. This condition is most commonly found on the left side due to anatomical differences in vein structure, which make the left testicular vein more vulnerable to pressure buildup. Additionally, increased abdominal pressure or standing for long periods may worsen venous congestion in the scrotum.
Several factors may contribute to the development of this condition. Genetic predisposition, connective tissue weakness, or prior venous issues in other parts of the body may play a role. While the exact trigger is not always clear, lifestyle habits and physical exertion may exacerbate symptoms. Environmental factors such as heat exposure or tight clothing might also be contributing elements. Understanding the varicocele causes is key in both prevention and choosing the right treatment path. If you’re experiencing discomfort or fertility issues, identifying the root cause can help guide your healthcare decisions effectively.
Varicocele and Male Fertility
The relationship between varicocele and infertility is well-documented in medical literature. Varicocele can interfere with sperm production and function by increasing scrotal temperature and impairing oxygen supply to the testicles. These physiological changes create a less-than-ideal environment for healthy sperm development. Studies show that men with varicocele often present with decreased sperm count, motility, and morphology, all of which can significantly reduce the chances of natural conception. Addressing the varicocele may improve these parameters and enhance fertility outcomes.
If left untreated, varicocele can gradually cause damage to the testicular tissue, leading to hormonal imbalances and long-term reproductive issues. For couples experiencing difficulties conceiving, diagnosing and treating varicocele can be a turning point. In many cases, surgical correction leads to improved semen parameters and increased pregnancy rates. Patients should consult a fertility specialist to determine whether their varicocele fertility condition is affecting their reproductive health. Identifying the issue early and pursuing appropriate treatment options, such as assisted reproductive technologies, may significantly improve the chances of a successful pregnancy.
How Does Varicocele Affect Sperm Quality?
Varicocele can negatively impact sperm quality by disrupting testicular temperature regulation and blood circulation. These changes may lead to oxidative stress, which damages sperm DNA and reduces sperm motility and count. Over time, these effects contribute to reduced fertility potential. Identifying this issue early is crucial when assessing male factor infertility linked to varicocele and infertility conditions.
How To Treat Varicocele?
There are several effective approaches when considering how to treat varicocele, depending on the severity of the condition and whether it impacts fertility or causes pain. In mild cases with no significant symptoms, treatment may not be necessary and simple monitoring can be sufficient. However, when discomfort or infertility is present, medical intervention is often recommended. Common non-surgical options include scrotal support and lifestyle modifications like avoiding prolonged standing and reducing physical strain. Pain management may involve anti-inflammatory medications.
For more serious cases, surgical procedures such as varicocelectomy or percutaneous embolization are commonly performed. These techniques aim to block the faulty veins and redirect blood flow through healthy vessels. Both methods are minimally invasive and typically performed on an outpatient basis. Surgery can significantly improve sperm quality in men dealing with fertility issues. Before proceeding with any form of treatment for varicocele, a detailed evaluation by a urologist or fertility specialist is essential to determine the best course of action. Choosing the right treatment option can improve quality of life and increase the chances of conception.
Can Varicocele Go Away on Its Own?
Many individuals wonder can varicocele go away without medical intervention. The short answer is no—varicoceles do not typically resolve on their own. Since the condition stems from faulty valves in the scrotal veins that allow blood to pool, the underlying issue persists unless treated. While symptoms may temporarily lessen with rest or changes in activity, the structural problem within the veins remains. Ignoring a varicocele can allow it to worsen over time, potentially leading to increased discomfort, testicular damage, or fertility complications.
However, not all varicoceles require immediate treatment. If the varicocele is small, asymptomatic, and not affecting fertility, healthcare providers may suggest a watchful waiting approach. Regular check-ups and lifestyle adjustments, such as avoiding heat exposure and wearing supportive underwear, can help manage mild cases. That said, for men trying to conceive or experiencing symptoms, active treatment is often necessary. Consulting a specialist will help determine if intervention is required. Ultimately, understanding whether a can varicocele go away situation applies to you depends on medical evaluation and long-term reproductive goals.