Does hysteroscopy improve IVF success is one of the most frequently asked questions by individuals navigating the emotional and physical journey of assisted reproductive technology. IVF (in vitro fertilization) success rates can be affected by a wide range of factors, including the health and condition of the uterus. In this context, hysteroscopy has emerged as both a diagnostic and therapeutic tool that may uncover and treat conditions that interfere with embryo implantation.
Hysteroscopy IVF procedures have gained attention because they allow fertility specialists to identify and manage abnormalities within the uterine cavity that could reduce the chances of pregnancy. From polyps and fibroids to adhesions and subtle endometrial irregularities, hysteroscopy can help optimize the uterine environment for embryo transfer. As IVF becomes more common, so does the need to improve its effectiveness especially for those who have experienced repeated IVF failures or unexplained infertility.
What Is a Hysteroscopy?
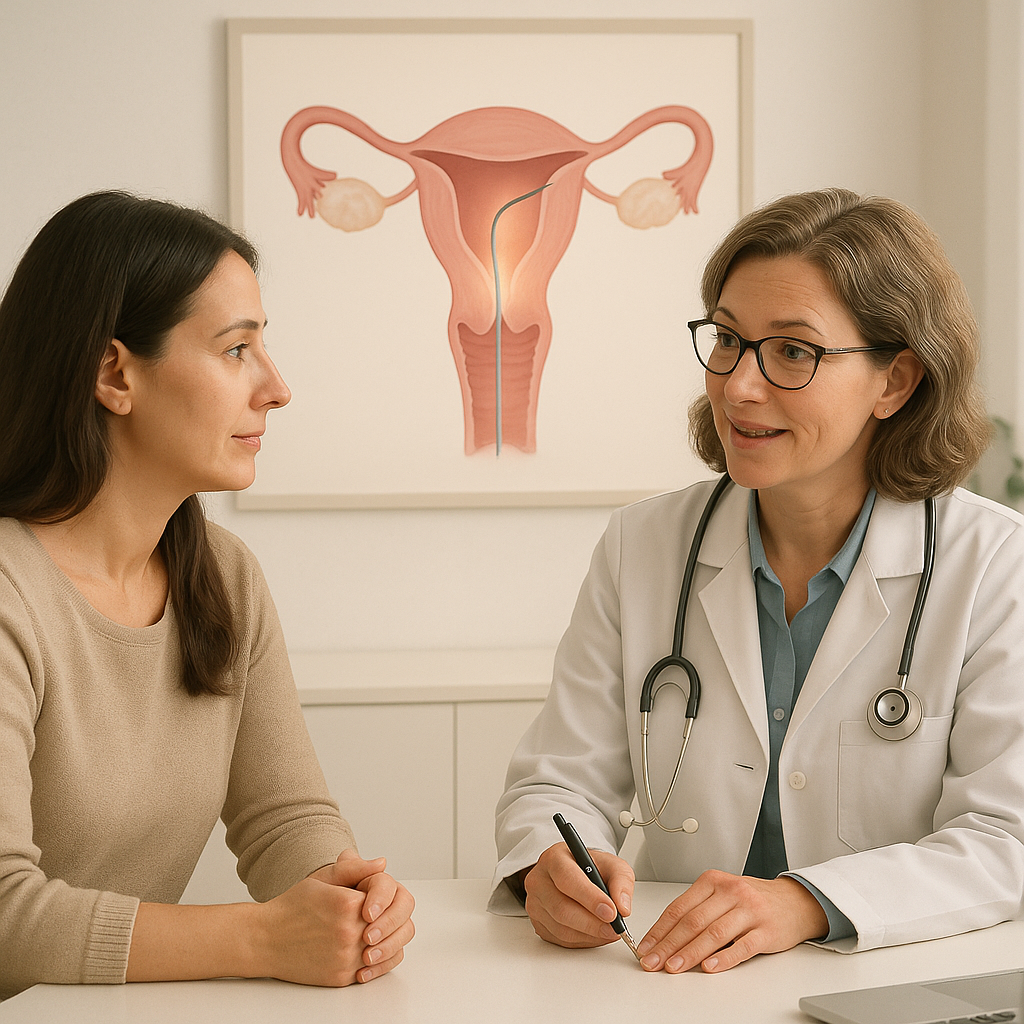
A hysteroscopy is a minimally invasive procedure that allows doctors to look directly inside the uterus using a thin, lighted telescope called a hysteroscope. The device is inserted through the cervix, which means there are no incisions, and it provides a clear view of the uterine cavity. This process helps detect abnormalities such as uterine polyps, fibroids, scar tissue, or any other structural issues that could impact fertility or pregnancy.
The hysteroscopy meaning varies depending on whether the procedure is diagnostic or operative. A diagnostic hysteroscopy is used solely to examine the uterus, while an operative hysteroscopy can treat issues on the spot by removing or correcting anomalies. Fertility clinics often use hysteroscopy before IVF to rule out or treat problems that may not be visible on ultrasounds or HSG (hysterosalpingography) tests.
Understanding what is a hysteroscopy helps patients feel more prepared and informed, especially when the goal is to improve IVF outcomes. It’s a fast, effective way to get a detailed understanding of uterine health and ensure the best possible environment for embryo implantation.
What Happens During a Hysteroscopy Procedure?
During a hysteroscopy procedure, the patient is usually placed in a gynecological position, and a hysteroscope is gently guided through the vagina and cervix into the uterus. The procedure can be done in a clinic or hospital setting, and depending on its complexity, it may require local anesthesia, conscious sedation, or general anesthesia.
Once inside the uterus, the doctor inflates the uterine cavity with a liquid solution to get a clearer view. The hysteroscope transmits images to a monitor, allowing the doctor to inspect the uterine lining for abnormalities. If any irregularities are found, such as polyps or fibroids, they can often be treated immediately using small instruments passed through the hysteroscope.
Knowing what is a hysteroscopy operation helps reduce anxiety for many patients. The entire procedure usually lasts between 10 to 30 minutes. Most individuals experience only mild cramping and can return to normal activities within a day or two. For IVF patients, this simple yet powerful diagnostic tool can make a significant difference in treatment planning.
When Is Hysteroscopy Recommended Before IVF?
Hysteroscopy is typically recommended before IVF when there’s a history of unsuccessful embryo transfers, abnormal uterine findings on ultrasound, or symptoms suggesting intrauterine pathology. For women who have experienced recurrent implantation failure or early miscarriages, hysteroscopy can offer critical insights into potential causes. Fertility specialists may also advise hysteroscopy if a prior imaging test like an HSG reveals abnormalities that require further investigation.
The goal is to ensure that the uterine cavity is free from structural or functional issues that may prevent successful implantation. In some cases, even in the absence of clear symptoms, hysteroscopy is used as a routine preparatory step for IVF, particularly in women over 35 or those with previous fertility treatments. The connection between hysteroscopy IVF planning and successful implantation has become increasingly recognized in clinical practice, making this procedure a valuable part of personalized fertility care.
Common Uterine Issues That Affect IVF Success
Several uterine conditions can significantly reduce IVF success, making it essential to identify and treat them before embryo transfer. Among the most common are endometrial polyps—small growths in the uterine lining that can disrupt embryo attachment. Fibroids, particularly submucosal ones that distort the uterine cavity, are another frequent culprit. These benign tumors may interfere with implantation or increase the risk of miscarriage.
Adhesions or scar tissue, often resulting from previous surgeries or infections, can partially or completely block parts of the uterine cavity. This can hinder embryo implantation or prevent it altogether. Hysteroscopy provides a direct view and allows for the accurate identification of these problems. Addressing these issues beforehand significantly improves the conditions within the uterus, thus boosting the likelihood of IVF success.
Diagnosing Polyps, Fibroids, and Scar Tissue
One of the key strengths of hysteroscopy is its precision in diagnosing uterine abnormalities that might not be detected through standard imaging techniques. What is a hysteroscopy useful for if not to identify and, in many cases, treat issues like polyps, fibroids, and intrauterine adhesions? These conditions are notorious for compromising the uterine environment, but their subtle presence often goes unnoticed without a thorough examination.
During hysteroscopy, any abnormal tissue such as polyps can be visually confirmed and removed in the same session. Fibroids can be evaluated for size, location, and impact on the uterine cavity, guiding treatment decisions. Similarly, scar tissue can be cut away to restore a normal uterine shape. By diagnosing and resolving these concerns, hysteroscopy contributes directly to improving the IVF success rate after hysteroscopy, especially in patients who previously failed to conceive without an obvious reason.
Role of Hysteroscopy in Unexplained Infertility
For couples dealing with unexplained infertility, hysteroscopy can uncover subtle uterine abnormalities that might not appear on ultrasounds or blood tests. Even in women with regular cycles and normal hormone levels, issues like a thin endometrial lining, hidden adhesions, or small polyps can hinder natural conception or IVF success. In such cases, hysteroscopy provides a deeper look into potential causes and offers a path for resolution.
This procedure often becomes the turning point in infertility investigations, especially when no other obvious causes are found. The ability to both diagnose and treat abnormalities in a single session makes hysteroscopy an efficient and minimally invasive option. When included as part of IVF preparation, it often shifts the outcome positively, offering renewed hope to couples previously left without answers.
IVF Success Rate After Hysteroscopy: What the Research Shows?
Numerous studies have explored the IVF success rate after hysteroscopy, and the results have been consistently promising, especially for patients with previously undiagnosed uterine abnormalities. Research has shown that treating intrauterine pathologies like polyps, fibroids, and adhesions significantly increases implantation rates and live birth outcomes. In fact, some studies suggest that even in women with a normal ultrasound, routine hysteroscopy before IVF can lead to improved pregnancy rates.
One meta-analysis revealed that women who underwent hysteroscopy before IVF had higher clinical pregnancy rates than those who did not. The greatest improvements were seen in patients with prior IVF failures. This evidence has led many fertility clinics to incorporate hysteroscopy as a standard part of the IVF preparation process, particularly for women over 35 or those with unexplained infertility.
It’s important to note, however, that results can vary depending on the patient’s age, overall fertility health, and the specific uterine issues identified and treated. But overall, when used appropriately, hysteroscopy has a positive impact on IVF outcomes and offers a valuable return on the physical and emotional investment of fertility treatments.
After Hysteroscopy: How Soon Can You Start IVF?
Once hysteroscopy is completed, many patients are eager to know how long after hysteroscopy can you do IVF. The answer largely depends on the findings and whether any surgical treatment was performed during the procedure. In most cases, patients can begin IVF treatment in the very next cycle—often about four to six weeks later—once the uterus has had time to heal and the endometrial lining has returned to a receptive state.
Timing is crucial in fertility care, and starting IVF too soon after hysteroscopy could compromise results if the uterine lining hasn’t fully recovered. On the other hand, waiting too long could delay the treatment unnecessarily. Fertility specialists usually base this decision on the individual’s medical history, age, and whether any abnormalities were corrected during the procedure. For example, after polyp or fibroid removal, a short healing period is generally sufficient before moving forward with the IVF protocol.
Recovery Time and Uterine Healing
The recovery time after hysteroscopy varies, but most women experience only mild discomfort and can return to regular activities within 24 to 48 hours. If the procedure was purely diagnostic, recovery is almost immediate. However, if surgical treatment was involved—such as removal of fibroids or adhesions—the healing process may take a few weeks. It’s essential that the uterus is fully healed before starting IVF to ensure a healthy and receptive environment for embryo implantation.
During this time, fertility specialists may recommend medications or supplements to support endometrial health. They may also perform follow-up ultrasounds or a second-look hysteroscopy to confirm that the uterine cavity is in optimal condition. Proper post-procedure care improves not only physical recovery but also increases the chances of a successful IVF outcome.
Typical IVF Timeline Post-Hysteroscopy
A typical after hysteroscopy IVF timeline begins with rest and monitoring for any signs of infection or complications in the first week. If everything looks normal, the patient may begin ovarian stimulation in the following menstrual cycle. This is usually between four to six weeks post-procedure. The IVF process—ovarian stimulation, egg retrieval, fertilization, and embryo transfer—follows the standard course unless adjustments are needed based on the hysteroscopy findings.
Doctors might modify the IVF protocol based on what was discovered during the hysteroscopy. For example, in cases where endometrial healing is critical, embryo transfer might be delayed, and embryos frozen for use in a future cycle. This approach allows for maximum uterine recovery and improves implantation success. Overall, careful planning post-hysteroscopy ensures the best use of IVF resources and maximizes the patient’s chances of conceiving.